A 55 years male patient with history of sudden abdominal pain followed by syncope was rushed to the hospital. CT abdomen + angiogram s/o fusiform dilatation of the abdominal aorta. Eccentric thrombus along the left lateral wall, showing further extension along the aortic bifurcation to involve bilateral common iliac arteries may represent thrombosed aneurysm/ intramural hematoma.
The findings most likely represent a ruptured & thrombosed fusiform aortic aneurysm. On receiving patient in ICU he was in hypovolemic shock with poor general condition. Blood pressure on admission was 80/40 mmHg, with a heart rate of 120/min. Physical examination of the abdomen was soft with tenderness in the left lower quadrant. No pulsatile mass was present. Femoral pulses were palpable symmetrically. Nor Adrenaline infusion started. Routine investigations sent and volume resuscitation was done with Blood transfusion followed by Fresh Frozen Plasma. Hb was 6.5 with an INR of 1.2. Rest routine reports were within acceptable range.
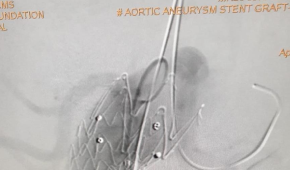
Patient was stabilized and shifted to Cath Lab for Abdominal Aortic Stenting.
She underwent Abdominal Stenting with Graft by a team of Interventional Radiologists & Cardiologists. Post procedure PCV transfused with Hb of 8.0. There was no further drop in Hb and rest of hospital stay was uneventful and patient discharged on POD 5.