
Cardiac Resynchronization Therapy is a treatment option in which a device is inserted in the heart which enables the heart, especially its lower chambers to pump blood better into the body. A biventricular pacemaker is inserted which helps both the ventricles to pump blood at the same time in a coordinated manner.
CRT is done mainly in cases of heart failure, when the pumping capacity of the lower chambers is impaired. Additionally, some CRT devices have an implantable cardioverter defibrillator (ICD) which can help revert life-threatening heart rhythms to normal state.
CRT is recommended for patients of heart failure with NYHA Class III or IV who remain symptomatic despite optimal medical management, with prolonged QRS and left ventricular heart function below 35%. In patients who need pacemaker for other indications and have heart function less than 50%, they can also be considered for CRT device as well.
Diagnostics
Patients should be thoroughly worked up prior to consideration for CRT implantation. Routine blood tests are done. ECG is done to document a prolonged QRS duration and a detailed Echocardiogram is done. Heart failure medicines should be fully optimized. Coronary angiography is usually done in most patients to rule out any significant blockages in the heart arteries. Sometimes cardiac MRI may be done to rule out causes of impaired heart functioning.
CRT, as mentioned previously, is done in patients of impaired heart functioning (LVEF less than 35%), whereas, ICD is inserted for patients having history of (or having high risk of) abnormal life threatening heart rhythm in the form of ventricular tachycardia or fibrillation.
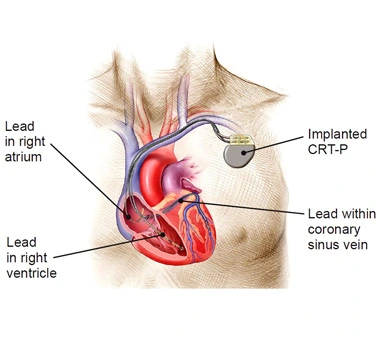
If patients have a high risk of ventricular tachycardia and their heat pumping is low, then may qualify for a combined device of CRT and ICD called CRT D (CRT plus defibrillation). If only CRT is needed it is also called as CRT P (CRT plus only pacing).
Patient and relatives are counselled about the procedure thoroughly including the procedure details, risks and benefits, and subsequently an written informed consent is taken.
Patient is taken to the cath lab. Local anaesthesia is given below the left collar bone. A linear incision is made parallel to the collar bone and a pocket is created between the skin and the muscles of the left chest.
Fluoroscopy or ultrasound guided punctures are taken to enter the subclavian or axillary veins. Cardiac leads are placed under fluoroscopy in the right ventricle (lower chamber), left ventricle via the coronary sinus and also in the right atria (upper chamber). Then a battery is inserted just under the collar bone beneath the skin, where the pocket was made and leads are connected to the same.
Thereafter the device is checked on the table to see if its parameters are adequate. If found satisfactory, the skin is closed with sutures or staplers. Patients are usually observed in the ICU overnight and discharged in 1-2 days post procedure.
Post-procedural Care and Monitoring
Immediate post-implantation care
These patients are shifted to the ICU and X ray of chest is done to see for any injury to the heart or lungs and to see the lead positioning. Antibiotics are also continued for a few days to prevent infections.
Long-term follow-up and device monitoring
CRT insertion patients have to be under lifelong surveillance. At least yearly follow up and device check needs to be done. Heart failure medicines need to be titrated as needed. If patients have new symptoms or observe fever or swelling at the device site, they should immediately see the doctor.
Early Complications
Late Complications
CRT devices have good evidence of improving the symptoms of the patients. Many patients have improvement in heart function post device insertion. With this not only the quality of life is better, but also the survival rates are improved.
Challenges and Limitations of CRT
Patient selection is paramount in CRT insertion. If indications are not right, the improvement post CRT insertion is questionable. Long term management and device checks are needed for these patients. Cost is also an understandable issue and also the doctors have to be duly qualified to do these procedures to give best possible outcomes and least complication rates.
CRT in Patients with Comorbidities
There are no alarming contraindications for CRT implantation. If the indication fits in and we expect that patients may live for more than a year, we can offer them CRT devices to aid in treating heart failure better in these patients.
