A 67 years old male patient with a history of dyspnoea of exertion since 1 month which worsened since 15 days. He was diagnosed with severe Aortic Valve Stenosis.
Vitals Stable
CVS – EFM Systolic Murmur
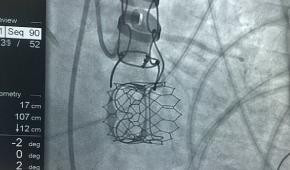
He underwent TAVI (Trancatheter Aortic Valve Implantation) under local Anaesthisia + Sedation by Dr. Ankur Phatarpekar and his team through right femorial artery.
Post procedure was shifted to ICU with stable Haemodynamic for observation.
Post procedure ECG sinus rhythm no ST-T changes.
After 24hrs left femorial sheaths were removed.
He was mobilised out of the bed.
Beta Blockers with held in view of Borderline Bradycardia.
Post Procedure Echo Screening.
2D-Echo – Gross Concentric LVH. All chambers normal size. Mild and distal septum mildly hypokinetic. Heavily calcified Aortic valve with reduced opening with peak by mean gradient of 86/53 mm of Hg suggestive of Severe AS with Grade ¼ AR. Grade ¼ MR, Grade ¼ AR. No evidence of PR/TR. No significant gradient across LVOT/RVOT. Normal LVEF – 61%
2D-ECHO- Normal LV systolic function. k/c/o degenerative Severe AS , s/p TAVI with normally functioning of Aortic valve. Mild Concentric LVH. All chambers normal size.
Bioprosthetic Aortic valve in situ, opening well. No e/o paravalvular leak.
Grade I MR. No evidence of AR/PR/TR. Peak by mean gradient across Aortic valve is 28/16 mm of Hg. AVA by continuity is 1.43 sq.cm.
LVEF 65%.
Right femorial and left femorial artery venous punctured.
Left femorial side 6-F sheath introduced in both venous and artery.
Right common femorial artery 10-F sheath introduced.
23 size balloon used for commissurotomy and inflated for 3 seconds.
Ventricle with pacing at 180 beats/min gradiant aortic valve – nil.
Following commissurotomy 23 size MyVal pericardial, bioprothes crimpel introduced and implanted across aortic valve with ventricular pacing of 180 beats/min.
No para valvular leak.
Good result.
Right femorial cannulation closed with proglide.
2 proglide used.
Good haemostasis.
Patient tolerated procedure well.