
Medically Reviewed By Dr. Meghav Shah Updated on August 1, 2024
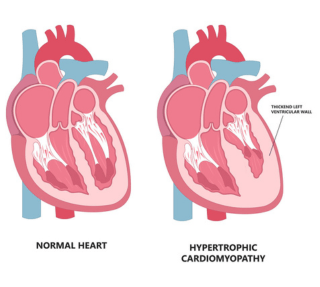
HCM is a condition in which the heart muscles in the lower chambers, i.e. the ventricles get abnormally thickened. The thickness is most often in the septal region i.e. the wall separating the two ventricles. Occasionally, it can also have thickening in the apex of the left ventricle or the right ventricle too.
This condition can hamper the flow of blood from the heart into the aorta or impair the filling of blood in the ventricles, thus can cause symptoms because of the same.
Basically, HCM is of 2 broad types, obstructive (70%) and non obstructive (30%). When there is obstruction in the outflow tract of left ventricle (LVOT) i.e. gradients when blood flows from the LV into the aorta, it is called HOCM i.e. hypertrophic obstructive cardiomyopathy. If there is no obstruction in the LVOT, it is called HCM i.e. Hypertrophic cardiomyopathy.
How it affects the Heart Function?
As mentioned previously, HCM results in thickening of the muscles, most commonly in the septum of the ventricles. This causes the heart to become slightly stiff over the time, causing impaired filling or relaxation of the ventricles, causing symptoms of shortness of breath or fatigue or chest pain.
In addition to it, if it is an obstructive variant, there is, as the name suggests, obstruction in the blood flow from the heart into the body and that can also result in dizziness or syncope and falls.
HCM is the most common hereditary disease of the heart and can affect around 0.1-0.2% of the general population.
It is usually inherited as an autosomal dominant condition with variable penetrance. Mutations of more than 25 genes have been identified as to the cause of this condition.
It can run in families, and thus if a patient is diagnosed with HCM, it is imperative to screen immediate family members for the same.
This condition can be asymptomatic or it can cause symptoms which can significantly impair day to day life of the patient.
Patients can complain of -
Many times, this condition may be diagnosed incidentally when a ECG or Echocardiogram is done for some other indications.
ECG - can show changes of left ventricular strain pattern with abnormal T wave inversions in septal and lateral leads. A normal ECG cannot exclude HCM.
Echocardiogram - can show septal thickening or hypertrophy and can also measure the gradient in the LVOT into the aorta. It can also quantify the impaired filling i.e the diastolic dysfunction and finally in later stages identify drop in the systolic function of the heart as well. In some cases, provocative tests in the form of giving some medications or valsalva maneuvers can be done to induce gradients in the LVOT to diagnose obstructive variants of HCM.
Cardiac MRI - can be done in some patients to look for scarring the ventricles or to quantify the exact thickening of septum or to diagnose atypical variants of HCM.
Holter Monitoring - can be sometimes done to detect abnormal heart rhythm in the form of ventricular tachycardia or atrial fibrillation.
In most cases, no treatment is needed if the patient is asymptomatic.
Medications
Rate control in the form of mainly beta blockers, verapamil or diltiazem. This improves the time for the ventricle to fill in HOCM, patients should avoid medications that can reduce preload or afterload like nitrates, diuretics, etc.
Surgery
Alcohol Septal Ablation is done in select cases to reduce the septal hypertrophy by intentionally causing a localized ischemia in the septal area. This procedure is done percutaneously through the groin arteries.
Septal Myectomy is performed in some cases resistant to optimal medical management and are not considered good candidates for alcohol septal ablation. This is carried out by surgeons via open heart surgery.
ICD i.e internal cardiac defibrillator device insertion is also advised in some patients who are found to be at increased risk of sudden cardiac death.
If left untreated it can cause worsening of symptoms. It can also cause drop in systolic dysfunction with lowered left ventricular pumping capacity if untreated for a long time. If this occurs there are more pronounced symptoms of heart failure. Sudden cardiac death can also occur in these untreated patients.
Conclusion
HCM is a common yet not frequently diagnosed genetic heart condition that can have a varied spectrum of presentation, from being asymptomatic to having symptoms of heart failure to having sudden cardiac death. Thus general awareness for this condition is paramount and once diagnosed, these patients should regularly follow up with their physicians and take appropriate medicines and if need be, should undergo ICD insertion or have surgical procedures as advised by their doctors.