
Medically Reviewed By Dr. Meghav Shah Updated on November 28, 2024
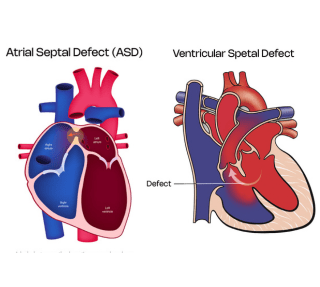
Normally both the right and left atria i.e. the upper heart chambers are separated by an interatrial septum and the ventricles i.e. the lower heart chambers are separated by an interventricular septum. Any defect in these membranes is called septal defects.
Normally, the blood in the right side of the heart has deoxygenated (less oxygen) blood and the left side of the heart has oxygenated (more oxygen) blood. These septa normally prevent the mixing of the blood on the right side with the left side of the heart, thus maintaining the integrity of the normal blood circulation in the body.
Subtypes of ASD
Subtypes of VSD
These septal defects are congenital, i.e. people are born with them since birth.
Exact cause for same is not known, but it is due to varied genetic and environmental reasons.
Certain medicine intake or addictions like smoking or alcohol consumption in pregnancy can be a causative factor.
Many a times these defects may be a part of a more generalized syndrome disorder, for eg. Holt Oram Syndrome, Downs Syndrome etc.
Rarely, as mentioned previously VSD can occur secondary to massive heart attacks or by iatrogenic injury i.e. injury during some heart operations.
ASD
VSD
Medicines
Water tablets or diuretics are mainly for symptom relief if there is shortness of breath or swelling over the feet.
Occasionally beta blockers are given if there are symptoms of Palpitations or fast heart beating.
Also, in certain cases, medicines may be given to reduce the pressures in lungs.
Definitive Procedure
If amenable via percutaneous device closure i.e. putting a device through the groin arteries to close the defect is the preferred procedure. It can be done occasionally without general anesthetic as well. If successful, patients are discharged home the next day.
If device closure is not possible, then an open heart surgery can be done to close the defect.
If untreated, these defects can cause irreversible damage to the heart and lungs called as Eisenmenger syndrome, and if this gets established these defects are deemed inoperable.
This occurs because there is increased blood flow to the right heart chambers because of the defect and subsequently more blood flows into the lungs. Over the time secondary to increased blood flow in lungs, the pressures in the lungs increases and this raised pressures becomes irreversible even when the defect is closed. On the contrary it may be of more harm than good if defects are closed post Eisenmengerisation.
These patients have a very poor quality of life, they turn blue secondary to more deoxygenated blood flowing in the body, are very lethargic and short of breath and have gross swelling over the feet.
ASD and VSD are usually congenital defects and need to be identified and treated early. Any child complaining of tiredness or shortness of breath should see a child physician and if deemed likely to have these conditions, they should be referred for an Echocardiogram. If diagnosed on same, these patients should be referred to pediatric cardiologists for consideration of closure in the form of Percutaneous device closure or open heart surgery.