
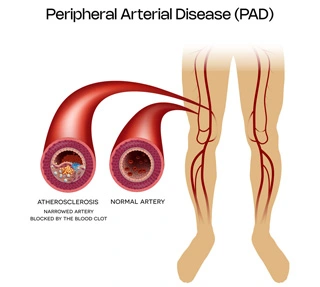
The most common cause is atherosclerosis. Atherosclerosis means the hardening of the arteries and formation of plaques or clots in these vessels. This can be due to old age and high lipidl evels/cholesterol levels or due to smoking.
Risk factors for atherosclerosis/PVD include:
A clinical examination is key. Screening tests for detection include a test called ABI - Ankle Brachial Index, where blood pressures in your arm and leg are compared.
Confirmatory tests include a Colour Doppler - to confirm the diagnosis.
For confirmation of the extent of blockage and the percentage and number of involved vessels an angiography is needed. This can be either a CT angiography, MR Angiography or a conventional invasive angiography also called DSA or Digital Subtracted Angiography.
Since PVD is a multi-system systemic problem, other vessels of your body may be blocked. 1/3rd patients may have blockages in the heart vessels. Therefore, an ECG and a 2D echo for heart function may be requested.
A quick arterial assessment called arterial Screening may be suggested. This would include a Carotid Doppler (to look for blockages in your arteries supplying the brain) as well as an Aortic Screening (to look for any associated aortic aneurysms AAA or aortic blockages).
Asymptomatic PVD patients may not require any treatment. Blood thinners and a few medications may have to be added to make sure there is no disease progression. This would ideally include Ecosprin and sometimes a low dose anticoagulant like Rivaroxaban may be added.
Claudicants may be treated in two ways. For lifestyle non limiting claudicants, conservative management may be tried with blood thinners and with exercise programs.
For lifestyle limiting claudication, intervention may be suggested depending on the level of blockage. For short blockages stenting or drug coated balloon angioplasty may be advised. For more complex lesions and blockages, bypass surgery may be suggested. This varies from case to case and treatment is tailor made depending in multiple clinical parameters.
Sometimes both surgery and stenting may be combined called “hybrid procedures.” For critical or acute limb ischemia, revascularization to improve the blood flow is essential. This generally involves angioplasty and/or stenting and sometimes combined with a bypass. This requires admission and is followed by a surgical clean up of the wound or ulcer and may sometimes also require an amputation.
Angioplasty/Stenting for Peripheral Vascular Disease
For patients with PVD, you may require to continue your blood thinners life long. It is important for correct foot wear. Wear closed shoes at all time. Socks to be worn at home to prevent wound or hurt to the leg. Prevent extreme hot or cold temperature to the legs to prevent boils and blisters. Any wound to the leg may not heal due to poor blood supply and may end up turning black due to “gangrenous” changes. A dedicated Foot Care regime needs to be followed as a lifestyle modification.
